 “Sibelle Yuksek shows off after getting her first dose of the Pfizer mRNA vaccine at the Union Station vaccine site in Los Angeles. Pfizer just announced it would seek emergency use authorization from the Federal Drug Administration for a third booster shot. Irfan Khan/Los Angeles Times via Getty Images
“Sibelle Yuksek shows off after getting her first dose of the Pfizer mRNA vaccine at the Union Station vaccine site in Los Angeles. Pfizer just announced it would seek emergency use authorization from the Federal Drug Administration for a third booster shot. Irfan Khan/Los Angeles Times via Getty Images
On July 8, pharmaceutical giant Pfizer announced it plans to seek emergency use authorization from the U.S. Federal Drug Administration (FDA) for a booster dose of its mRNA COVID-19 vaccine, citing the emerging delta variant and evidence of waning immunity in patients who had received the first two doses.
Almost immediately, the U.S. Centers for Disease Control and Prevention (CDC) and FDA released a joint statement shutting Pfizer down.
"People who are fully vaccinated are protected from severe disease and death, including from the variants currently circulating in the country such as Delta. People who are not vaccinated remain at risk. Americans who have been fully vaccinated do not need a booster shot at this time," the joint statement says.
So if you’ve been vaccinated against COVID-19, whether you got the Pfizer, Moderna or the Johnson & Johnson shot, you might be confused by these mixed messages — and wondering what a booster shot even is and whether you need one? Here’s what we know.
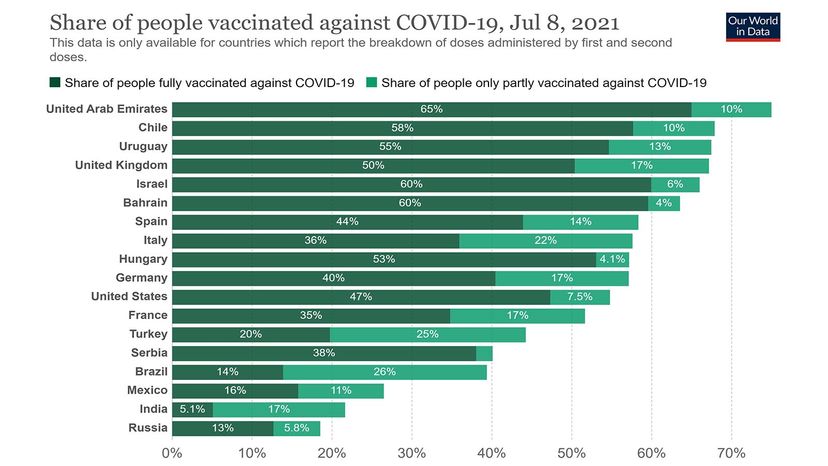 “This bar chart shows the share of people worldwide fully vaccinated and partially vaccinated against COVID-19 as of July 8, 2021. Official data collated from Our World in Data.Our World in Data
“This bar chart shows the share of people worldwide fully vaccinated and partially vaccinated against COVID-19 as of July 8, 2021. Official data collated from Our World in Data.Our World in Data
What Is a Booster Shot?
Booster shots are vaccinations given long after the initial injection to "boost" immunity. Some vaccines require booster shots, while others do not. For example, the yellow fever vaccine is a one-and-done; a single dose conveys immunity for life. On the other hand, whooping cough requires two vaccines — DTaP and Tdap. Children under age 7 get DTaP and children older than 11, teens and adults get Tdap. But why are these types of booster shots necessary in the first place?
"One of the explanations has to do with how the vaccine is actually formulated," says Dr. Amesh Adalja, a senior scholar at Johns Hopkins University Center for Health Security. The yellow fever vaccine uses a live, weakened — or attenuated — virus to trigger an immune response without causing illness. The whooping cough vaccine introduces tiny bits of bacterial protein, which don’t produce as strong of an immune reaction and might need to be reintroduced later.
"Aging is also a part of it," Adalja says. As people age, their immune systems naturally weaken over time. Vaccine protection acquired early in life can gradually wear off as a result.
So, with that in mind, how do the COVID-19 vaccines stack up in terms of effectiveness so far?
 “Tokyo Olympic organizers announced July 8 that spectators would be barred from most events at the games after a new state of emergency was announced in response to a surge in coronavirus cases. Japan has fully vaccinated less than 17 percent of its population as of July 9, 2021. Takashi Aoyama/Getty Images
“Tokyo Olympic organizers announced July 8 that spectators would be barred from most events at the games after a new state of emergency was announced in response to a surge in coronavirus cases. Japan has fully vaccinated less than 17 percent of its population as of July 9, 2021. Takashi Aoyama/Getty Images
The Life of a COVID-19 Vaccine
"They’ve been quite effective," says Dr. Rachel Presti, medical director of the Infectious Disease Clinical Research Unit at Washington University’s School of Medicine in Saint Louis, Missouri.
When it comes to COVID-19 vaccines, there are three major technologies from which to choose. Both the AstraZeneca and Johnson & Johnson vaccines use a weakened, slightly modified version of a common cold virus to trick the body into mounting an immune response. The Novavax shot uses the coronavirus’ own spike proteins against it, while Moderna and Pfizer use mRNA technology to train cells to recognize and attack the virus.
Presti has been researching the longevity of the protection conveyed by the Pfizer mRNA vaccine. So far, despite Pfizer’s claims, the results have been encouraging. "Even in people who were vaccinated back in December, we’re not seeing them coming down with severe infection," she says.
Truthfully, it may be a while before we know for sure whether COVID-19 booster shots are necessary. Experts will need to carry out long-term natural history studies, checking in on vaccinated participants to see how their immunity changes over many years. If their COVID-19 immune response decreases enough over time, an extra dose might be needed for lifelong protection.
Then there are variants to consider. As Pfizer pointed out, the delta variant is quickly becoming the dominant strain of COVID-19, and some scientists worry that a new mutation might render the current vaccines less effective. But that doesn’t necessarily mean that that vaccinologists will need to tweak the formula in the future.
"Even if you don’t reformulate the booster," Adalja says, "just giving a third dose of a two-dose vaccine against COVID-19 may provide enough immunity."
 “Mixing-and-matching, or heterologous, vaccines is nothing new. And while it’s probably too early to know whether we can mix-and-match COVID-19 vaccines like these (l-r) Biontech, AstraZeneca, Johnson & Johnson and Moderna, experts say the answer is probably yes.Marcus Brandt/picture alliance via Getty Images
“Mixing-and-matching, or heterologous, vaccines is nothing new. And while it’s probably too early to know whether we can mix-and-match COVID-19 vaccines like these (l-r) Biontech, AstraZeneca, Johnson & Johnson and Moderna, experts say the answer is probably yes.Marcus Brandt/picture alliance via Getty Images
Can We Mix and Match Vaccines?
What happens if you need a booster but can’t get the same type of shot as your initial dose? Is it OK to mix and match?
While it’s a bit too early to say for sure, the answer is probably yes. Mix-and-match, or heterologous, vaccines are nothing new; in fact, they can sometimes give better protection than single formulation shots. "I think probably the best example of that is the pneumococcal vaccine," Presti says.
There are "two different flavors" of pneumococcal vaccine, Presti explains, both of which protect against pneumonia. The booster vaccine is formulated differently than the initial dose. Shot No. 1 is more effective for kids, while shot No. 2 offers better protection for older folks. And the two vaccines are sometimes given jointly to individuals with autoimmune disorders.
Since different COVID-19 vaccines use different mechanisms to confer immunity, the theory goes there is a chance that mixing up the formulations might round out and strengthen the body’s overall response — think of it like two instruments playing in harmony.
One preliminary study from Spain found that people who received an AstraZeneca shot followed by a Pfizer produced a whopping 37 times more antibodies than with an AstraZeneca jab alone. And while most people probably won’t need that level of protection, it could prove lifesaving for immunocompromised folks.
The National Institute of Allergy and Infectious Disease (NIAID) recently launched its own clinical trial investigating the potential need for COVID-19 booster shots and the effectiveness of heterologous vaccines.
Welcome to the "Golden Age of Vaccinology"
The good news is that vaccine technology is getting exponentially better. Recent breakthroughs have enabled scientists to develop a several highly effective COVID-19 vaccines in record time. Even older shots are getting a makeover: Moderna just announced July 7, 2021, trials for its new mRNA influenza vaccine, which promises to offer longer lasting immunity against seasonal flus. Between these advances, Adalja suspects we might be on the cusp of a "Golden Age of Vaccinology."
So where does that leave the booster shot discussion?
If it’s a matter of completely preventing disease, "getting another dose is going to give you more antibodies," Presti says.
But, "when we’re talking about COVID-19," Adalja says, "it’s less about driving cases to zero. It’s about removing the ability of the virus to cause serious disease, hospitalization and death." For that, he says, a booster might be overkill.
Now That’s Interesting
Louis Pasteur developed the first lab-produced vaccine in 1879; it was used to immunize chickens against cholera. So, more of a rooster shot than a booster shot.

































