With Hurricane Laura hitting Louisiana and Texas as an “extremely dangerous” Category 4 storm and wildfires menacing the western U.S., millions of Americans faced the complex risks of a natural disaster striking in the middle of a pandemic.
The steps people normally take to prepare for a severe storm or to evacuate can contradict the public health recommendations for protecting themselves and others from COVID-19. That’s what millions of people were facing as Hurricane Laura intensified in the Gulf of Mexico. More than half a million people were under evacuation orders, including the cities Galveston, Beaumont and Port Arthur, Texas.
My urban resilience lab at Texas A&M University has been examining interactions between urban infrastructure, systems and people in disasters. At the onset of the COVID-19 pandemic, we launched a study into the effect of the pandemic on urban systems during a natural disaster, applying similar methods we used during extensive research on Hurricane Harvey, which flooded Houston in August 2017.
Our research shows that compound disasters have complex ramifications. At the intersection of a natural hazard and a pandemic is a decision process fraught with contradictions.
Storm prep and evacuations raise the risks
During the three days before Hurricane Harvey hit, the number of grocery store and gas station visits in the Houston area increased by 50% to 100%. People didn’t think twice about running to the store.
As Hurricane Laura headed for the Louisiana and Texas coasts, residents were in very a different situation. The rise of COVID-19 illnesses and deaths across the South during the summer meant people were encouraged to self-quarantine and limit their social contact to prevent transmitting the coronavirus. They could still wear masks in stores, but keeping the recommended six feet apart gets harder when stores get crowded. It means spending more time waiting with others in lines and jostling in the aisles. Research shows that both the amount of virus and the amount of time a person is exposed to it have an impact on whether they get infected and how severely.
An even more onerous complication – for both authorities and residents – is evacuation.
The decision to evacuate in the face of even a single hazard, whether a wildfire or a hurricane, is difficult. Sheltering in place can mean life-threatening conditions, prolonged power outages and disrupted access to critical facilities. Evacuating means leaving behind one’s house and possibly animals to an uncertain fate.
That’s complicated further when an emergency shelter is the best choice, but staying in one can mean a higher risk of being exposed to someone infected with the coronavirus.
Which areas are most vulnerable?
Authorities assess many variables when deciding between mandatory and voluntary evacuations. In the face of a pandemic, they now also have to think about disease transmission – and not just in individual emergency shelters but also on a larger scale. When a large population moves from an area with a high rate of disease spread to a less affected area, it can put the local population at higher risk.
Using data on social vulnerability, pandemic risk and hazard probability, my lab created an interactive map that pinpoints sources of vulnerability. The goal is to enable disaster response managers and decision makers to recognize the compound risks posed by the confluence of the pandemic and any natural hazard.
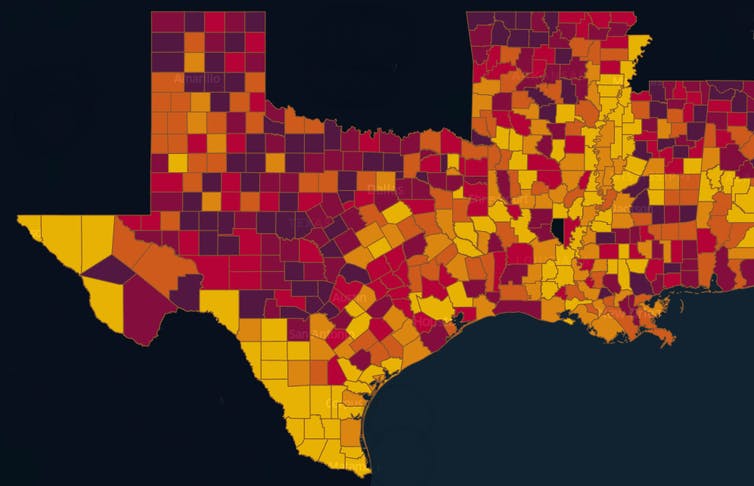
Texas A&M UrbanResilience.AI Lab, CC BY-ND
The compound hazard risk index takes into consideration the social, physical and pandemic risks at the local level, enabling each county or community to make informed decisions. It also raises warnings about vulnerable groups, such as the elderly and low-income communities, which may suffer a disproportionate risk of infection.
We found several counties with significantly high levels of compound risks.
For example, Harris County, Texas, home to Houston, has a large number of COVID-19 cases and is also vulnerable to the impacts of hurricanes. When a hurricane heads for the region, the index can help raise red flags, particularly for local health officials and hospitals, about the risks of exacerbating the pandemic there and in counties where people may go in an evacuation.
Conversely, a county with low hurricane and flooding risks might normally be seen as a suitable location for evacuation, but if it has a high rate of COVID-19, that raises the risk for evacuees who would need to spend time in shelters, hotels, restaurants and stores.
Getting health care can also become harder during a natural disaster. Hospitals may see an influx of injuries, and wildfires and flooding can block access to critical health care facilities, damage the buildings, cut power to homes and care facilities and shut down pandemic testing locations.
Other researchers have also explored the potential for an evacuation spreading COVID-19. In a recent study of evacuation patterns and COVID-19 cases in Florida, researchers at the Union of Concerned Scientists estimated that if a Category 3 hurricane hit Southeast Florida, the difference in that region between evacuees taking shelter in communities with low coronavirus transmission rates versus those with high rates could be as high as 50,000 new COVID-19 cases.
As our research shows, preparing for and responding to the compound disaster of a natural hazard in the midst of a pandemic is an undertaking more complicated than the sum of its parts.
This story was updated Aug. 27 with Hurricane Laura making landfall.
Ph.D. students Jennifer Dargin and Qingchun Li and undergraduate students Gabrielle Jawer, Sara Garcia, Xin Xiao, and Bora Oztekin contributed to the research on compound natural hazard and pandemic. Technical writer Jan Gerston contributed to this article.

































