Borderline personality disorder (BPD) is a complex, often misunderstood mental health condition. Mental health professionals used to think it was untreatable. But thanks to research in the last 30 years, we know it’s possible for people with BPD to benefit from specially developed talk therapies. (1)
At its most basic level, BPD is a disorder that causes a person to have impairments in self-identity and in regulating his or her emotions. People may go from one intense emotion to the next, feeling extremely loving followed by feeling irrationally angry. Once an event triggers a strong emotion, it’s harder for the person to return to a more stable state of mind. (2) These mood swings can last hours or days.
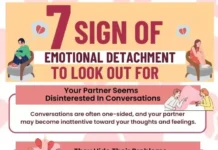
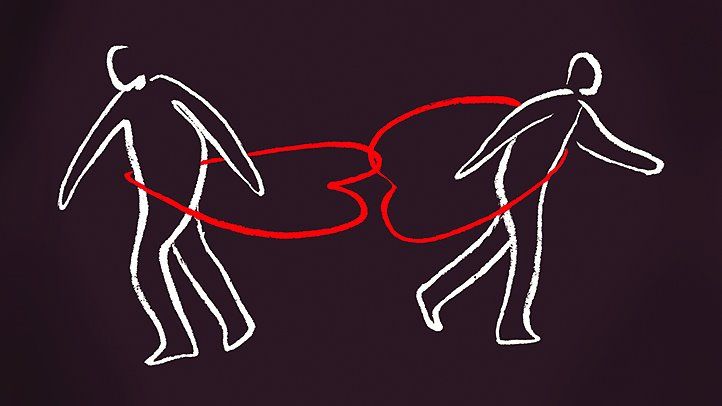
Such intense emotional responses can lead to trouble with personal relationships, self-esteem issues, and impulsive actions. (2) People with BPD may struggle with a fear of abandonment and find it difficult to be alone, but their actions and reactions can push people away. (3)
How Common Is BPD Exactly, and Does It Affect Women or Men More?
About 2 percent of American adults have BPD, but the number could be as high as almost 6 percent. (2)
From a diagnostic standpoint, it’s seemingly more common in women, people in lower-income communities, people younger than 30, and those who have been separated or divorced. (4) Around 75 percent of people diagnosed with BPD are women. (2) But men with BPD are more likely to be incorrectly diagnosed with depression, post-traumatic stress disorder (PTSD), or a different personality disorder, which could mean the number of men with BPD is higher than recorded.
Indeed, study results are conflicting: One survey in the Journal of Clinical Psychiatry suggesting that BPD actually affects men and women equally. (5)
A possible explanation for the higher percentage of women diagnosed could be gender bias in the diagnostic criteria, says Brittain Mahaffey, PhD, a clinical psychologist and research scientist at the Mind-Body Clinical Research Center at Stony Brook Medicine in Stony Brook, New York. Women are also more likely to be victims of abuse, she says, which can contribute to the development of BPD.
Learn More About the Prevalence of BPD Among Men and Women
What Are the Signs and Symptoms of BPD, and How Is It Diagnosed?
BPD causes people to experience intense emotions, which can make them feel insecure and cause them to act irrationally. This behavior is often seen in their relationships: Someone could be considered a close friend one day and an enemy the next day. (6)
“It’s really a relationship disorder — relationships can’t be functional, and that’s the trigger and pinpoint,” says Bethany Kassar, a licensed clinical social worker and the executive director of outpatient services at Summit Behavioral Health, based in New Jersey, Massachusetts, and Pennsylvania.
Signs and symptoms include: (2,3)
- An extreme, often irrational, fear of abandonment and extreme efforts to avoid experiencing it
- Intense, unstable relationships (going from extremely loving to cutting someone off completely)
- A negative self-image (thinking you’re bad or worthless) and an unstable sense of self
- Risky or impulsive behavior (drug abuse, unsafe sex, reckless spending, gambling)
- Self-harm through injury (for example cutting) or suicide attempts
- Severe mood swings that can last a few hours or a few days
- Having problems controlling anger and outbursts
- Frequently feeling bored or empty
- Feeling disconnected from thoughts or feelings
- Experiencing paranoia or loss of reality caused by stress
- Having a lack of direction (constantly changing goals)
Do You Have a Codependent Personality?
Anyone experiencing signs and symptoms of BPD should talk to a doctor about it. There isn’t a test or screening for BPD, so getting a diagnosis can take time and a careful evaluation. A doctor will meet with you to discuss symptoms and may also talk to your previous doctors or ask to interview friends and family about your behavior in relationships. (2)
BPD isn’t usually diagnosed in children because their personalities and traits are still developing, although experts do watch for signs early in adolescence. (7) Many people get a diagnosis in young adulthood, around age 18.
To diagnose BPD, a mental health professional (such as a psychiatrist, a psychologist, a therapist, or a licensed clinical social worker) will do the following: (6)
- Interview you and ask about your symptoms
- Discuss your family medical history (specifically if there’s a history of mental illness)
- Perform a medical exam to weed out symptoms of other conditions
Learn More About the Symptoms of BPD and How It’s Diagnosed
Causes and Risk Factors of BPD
Researchers still aren’t exactly sure why some people develop BPD and others don’t. It’s likely a combination of genetic, environmental, and neurological factors. (2,3)
- Family history People who have an immediate family member (parent or sibling) with BPD are more likely to develop it themselves. Research in twins has also shown a genetic link to the disorder. (2)
- Childhood trauma Many people diagnosed with BPD also experienced sexual abuse, neglect, or emotional trauma during childhood. (8)
- Brain structure The areas of the brain that help regulate emotion might be different in people with BPD. There may be either a chemical imbalance or a disconnect between the area of the brain that controls emotion and the area that makes decisions. For example, research suggests people with BPD have more trouble recognizing others’ facial expressions. (9)
Learn More About the Causes and Risk Factors of BPD
Is BPD Genetic? What to Know if You Have a Parent or Child With BPD
While there isn’t a single risk factor that leads to BPD, having a family member with the mental illness clearly can put you at an increased risk. According to the National Alliance on Mental Illness (NAMI), having a first-degree relative with BPD may put you at a more than fivefold increased risk. (2)
The same heightened risk can be seen among people with family members who have other personality disorders, research shows. (10)
But in a sense, family matters can affect your risk for BPD beyond genetics — there’s the environment during your upbringing that can play a role, too. For instance, abuse and neglect are tied to BPD. (11,12)
Similarly, growing up in a household with a parent who has BPD may create a chaotic environment that increases your risk of developing BPD in addition to the genetic risk that may be posed.
Learn More About How Genetics Can Play a Role in BPD Risk
What Are the Common Comorbidities of BPD, and How Does It Differ From Other Mental Illnesses?
It’s very common for someone with BPD to be diagnosed with other mental health conditions as well. In fact, about 85 percent of people with BPD also met the diagnostic criteria for another mental health condition. (13)
Common conditions also seen in people with BPD include:
- Anxiety
- Depression
- Eating disorders
- Post-traumatic stress disorder (PTSD)
- Phobia
- Substance use disorder or addiction
Unfortunately, these comorbidities share many of the same symptoms as BPD. “It’s a very hard diagnosis because it’s so complex,” says Kassar.
Without a proper background and medical history, someone can easily be misdiagnosed because the doctor is missing a piece of the puzzle. For example, people with BPD are often wrongly diagnosed with bipolar disorder based on irritability, impulsivity and anger management issues, according to Mahaffey.
Learn More About BPD Comorbidities and How Symptoms May Vary
What Are the Top Treatment and Therapy Options for BPD?
A treatment plan for BPD may include a few different approaches, but most often it will mainly consist of some type of talk therapy. (1,3) To help get the best results, it’s important to find a therapist who has experience with both BPD and the type of therapy you choose to receive. You’ll also want to work with someone you trust and feel comfortable with.
The goal of therapy for people with BPD is to learn how to deal with uncomfortable emotions, express needs and emotions in a healthy way, and improve relationships.
Common techniques used for BPD are:
- Cognitive behavioral therapy (CBT) The client works with an individual therapist to learn to identify negative thought patterns and view situations more clearly.
- Dialectical behavior therapy (DBT) DBT is a program specifically designed for people with BPD to teach coping skills for managing emotions and improving relationships. This can be done with an individual therapist or with a group.
- Mentalization-based therapy (MBT) The client learns to identify thoughts and feelings in the moment and think before reacting.
- Transference-focused therapy (TFP) The client works with an individual therapist to understand emotions and relationship challenges through the relationship developed with the therapist.
- Schema-focused therapy (SFT) Individual or group therapy helps the client recognize emotional needs that weren’t met earlier in life. The goal is to recognize how this led to unhealthy behaviors and learn healthy ways to get these needs met.
DBT is really the only intervention in wide use for BPD because it helps with basic emotion-regulation skills that people with BPD don’t have, says Mahaffey. (1)
There are no medications to treat BPD itself, but someone with BPD may be given medication to treat anxiety, depression, or mood swings. (2)
In some cases, a person with BPD might need hospitalization, particularly if they’re at a high risk for self-harm or suicide.
Learn More About the Best Treatments and Therapies for BPD
What Are the Consequences and Complications of Untreated BPD?
Aside from strained relationships, trouble with social interactions, and risk for job loss, untreated BPD can have dangerous consequences. People who don’t get treatment are at risk of harming themselves or attempting suicide, complications that can lead to hospitalization or even death. According to the National Institute of Mental Health, up to 80 percent of people with BPD have suicidal behaviors and about 4 to 9 percent commit suicide. (13)
“Usually self-harm serves the function of reducing emotional distress in people with BPD,” says Mahaffey. “People say it feels good or they get a sense of relief.”
There’s also the risk for exacerbating other mental illnesses that coexist with BPD.
Without the proper coping tools, which you can learn through therapy, it’s likely someone with BPD will continue to engage in self-harm or struggle with other symptoms.
Learn More About the Possible Complications of Untreated BPD.
Additional reporting by Jessica Migala.
Resources We Love


Editorial Sources and Fact-Checking
- Choi-Kain L, Finch EF, Masland SR, et al. What Works in the Treatment of Borderline Personality Disorder. Current Behavioral Neuroscience Reports. February 2017.
- Borderline Personality Disorder. National Alliance on Mental Illness. December 2017.
- Borderline Personality Disorder. Mayo Clinic. July 30, 2015.
- Tomko RL, Trull TJ, Wood PK, et al. Characteristics of Borderline Personality Disorder in a Community Sample: Comorbidity, Treatment Utilization, and General Functioning. Journal of Personality Disorders. October 2014.
- Grant BF, Chou SP, Goldstein RB, et al. Prevalence, Correlates, Disability, and Comorbidity of DSM-IV Borderline Personality Disorder: Results From the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. April 2008.
- Borderline Personality Disorder. National Institute of Mental Health. December 2017.
- Miller C. What Is Borderline Personality Disorder? Child Mind Institute.
- Statistics About Borderline Personality Disorder and PTSD. Borderline Personality Treatment.
- Anupama V, Bhola P, Thirthalli J, et al. Pattern of Social Cognition Deficits in Individuals With Borderline Personality Disorder. Asian Journal of Psychiatry. March 2018.
- Czajkowski N, Aggen SH, Krueger RF, et al. A Twin Study of Normative Personality and DSM-IV Personality Disorder Criterion Counts: Evidence for Separate Genetic Influences. American Journal of Psychiatry. March 2018.
- Ibrahim J, Cosgrave N, Woolgar M. Childhood Maltreatment and Its Link to Borderline Personality Disorder Features in Children: A Systematic Review Approach. Clinical Child Psychology and Psychiatry. January 2018.
- Fortaleza de Aquino Ferreira L, Pereira FHQ, Benevides AMLN, et al. Borderline Personality Disorder and Sexual Abuse: A Systematic Review. Psychiatry Research. April 2018.
- Post by Former National Institute of Mental Health Director Thomas Insel: What’s in a Name? The Outlook for Borderline Personality Disorder. National Institute of Mental Health. April 19, 2010.