Signs and Symptoms of Macular Degeneration
Macular degeneration doesn’t cause total blindness because it doesn’t affect peripheral vision. However, it can significantly interfere with daily activities — such as the ability to drive, read, write, cook, do certain chores, or recognize faces or colors.
It's also possible to have macular degeneration in only one eye, or to have a more severe form of the condition in one eye than the other.
The basic symptoms of macular degeneration are:
- Reduced or distorted central vision in one or both eyes
- Reduced ability to see or differentiate colors
- A blind or blurry spot in your field of vision
- General haziness in your overall vision
Visit your eye doctor if you notice changes in your central vision, or in your ability to see colors and fine detail — especially if you’re 50 or older.
As macular degeneration progresses, the blurred area near the center of your vision may grow larger, or you may develop blank spots in your central vision.
The initial symptoms of macular degeneration are not painful; and sometimes, when the condition begins in one eye, the stronger eye compensates, so you may not immediately notice changes in vision.
Stages of Macular Degeneration
Although macular degeneration in general, and AMD in particular, progresses more rapidly in some people than in others, there are three general stages:
Early AMD


How to Manage and Monitor Your Macular Degeneration
Intermediate AMD
Late AMD
In this stage, you develop medium to large drusen in your macula and, as a result, noticeable vision loss.
Types of Macular Degeneration
Age-related macular degeneration comes in two forms: dry (also known as geographic atrophy) and wet (known as neovascular, or abnormal blood vessel growth).
Dry Macular Degeneration
What Is Dry Macular Degeneration?
Wet Macular Degeneration
Stargardt Disease
How Is Macular Degeneration Diagnosed?
- A basic eye exam
- Amsler grid test
- Fluorescein angiography
- Optical coherence tomography
Basic Eye Examination
Amsler Grid
Fluorescein Angiography
Optical Coherence Tomography
Genetic testing may be used to identify young people at risk for Stargardt disease; eventually, scientists hope that a gene therapy approach might work to replace the defective genes that cause Stargardt or AMD, though this is likely several years into the future.
Prognosis of Macular Degeneration
If you develop early AMD, you may not progress to late AMD. Research shows that people with early AMD in one eye, and no signs of AMD in the other eye, have only a 5 percent chance of progressing to late AMD after 10 years.
Having late AMD in one eye does put you at increased risk for late AMD in your other eye. Having the condition in both eyes will likely impact your ability to read and perform other activities.
While there is currently no cure for any form of macular degeneration, available treatments may prevent severe vision loss or slow the progression of the condition.
Treatment and Medication Options for Macular Degeneration
Although there’s no cure for macular degeneration, several different approaches may be used to treat the condition and slow its progression.
Medication for Macular Degeneration
If you have wet macular degeneration, certain medications can stop growth of new, abnormal blood vessels in the macula. These drugs are called anti-vascular endothelial growth factor (anti-VEGF) therapies, and include Avastin (bevacizumab), Lucentis (ranibizumab), and Eylea (aflibercept).
The treatment, which may require repeated, monthly injections, has been shown to restore vision in some people with AMD, and prevent blindness in up to 90 percent of those who receive it.
If the treatment is effective, you may recover some lost vision as the blood vessels shrink and the fluid under the retina is absorbed.
Potential side effects include:
- Serious eye infections that may cause eye pain, light sensitivity, and vision changes
- Increased intraocular pressure, which can lead to glaucoma
- Retinal detachment
- Floaters (or shapes that appear in your field of vision)
Medical and Surgical Procedures for Macular Degeneration
A couple of noninvasive procedures may help with some forms of AMD:
Alternative and Complementary Therapies
The large study by the National Eye Institute called AREDS — the Age-Related Eye Disease Study — found that some people with AMD can reduce their risk for wet AMD and vision loss by taking vitamins C, E, beta-carotene, zinc, and copper supplements.
Learn More About Treatment for Age-Related Macular Degeneration
Prevention of Macular Degeneration
Certain steps can reduce your risk of developing macular degeneration and help manage your condition. This includes getting routine dilated-eye exams.
Make it a priority to quit smoking, since smokers are more likely to develop macular degeneration.
Research and Statistics: How Many People Have Macular Degeneration?
Approximately 11 million people in the United States are living with macular degeneration, research suggests. That number is expected to double by 2050, due to the aging population.
Related Conditions of Macular Degeneration
Macular degeneration is the leading cause of vision loss in people ages 50 and older. However, there are other eye conditions to watch out for as you age.
Cataracts
Cataracts aren't preventable, but they’re treatable with surgery.
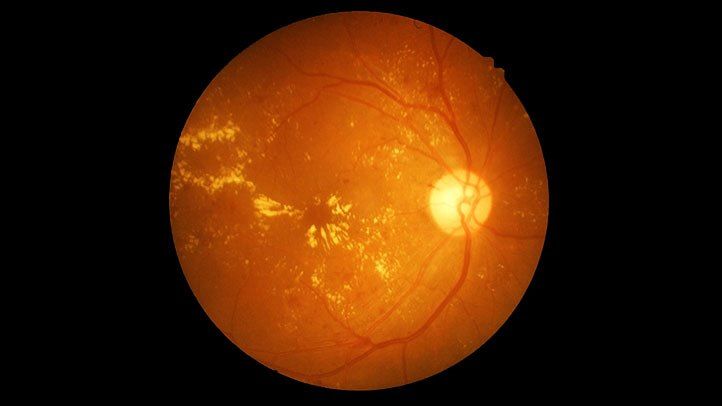
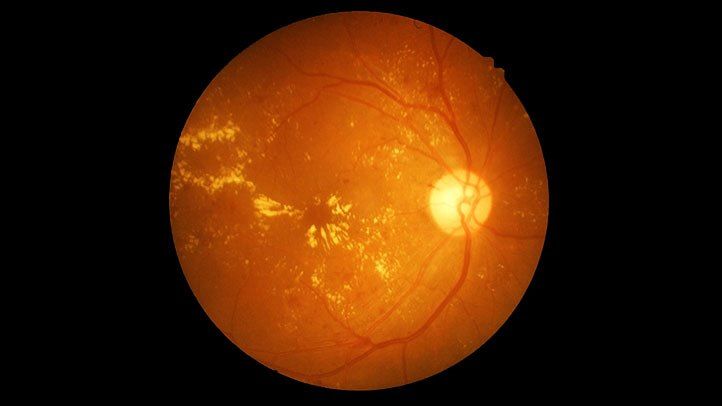
Diabetic Retinopathy
Diabetic retinopathy is a chronic condition caused by diabetes as a result of damage to the blood vessels of the light-sensitive area at the back of the eyes. At first the condition causes minor vision problems, such as difficulty seeing at a distance.
However, as diabetes progresses retinopathy does as well, and may eventually lead to blindness. Still, diabetic retinopathy can be managed with laser treatments and some patients may have vitrectomy surgery.
Glaucoma
Glaucoma is a collection of eye conditions that can eventually damage the optic nerve — usually as a result of increased pressure in the eye, or intraocular pressure. Glaucoma can lead to loss of peripheral vision and, over time, cause total blindness if it’s left untreated. It can be prevented by lowering intraocular pressure with topical eye drops or surgery.
Presbyopia
At about age 40, many adults develop a condition called presbyopia, which affects both near and distance vision. The condition can make daily activities — such as reading and working at the computer — challenging but, for most people, eyeglasses or contact lenses designed to address it can help.
Dry Eye
Older adults are also more prone to an eye condition called dry eye, which is caused by low tear production. People with dry eye don’t produce sufficient tears to keep their eyes well lubricated, causing discomfort, including redness, stinging, and burning, all of which may impact vision. There isn't a cure for dry eye, but saline lubricating drops or artificial tears can help to relieve some of the symptoms. Some prescription drugs can also help manage the condition.
In general, older adults with vision problems are 200 percent more likely to be involved in motor vehicle accidents, so it's important to be aware of how aging may affect your vision.
Additional reporting by Deborah Shapiro.
Resources We Love
Editorial Sources and Fact-Checking
- What Is Macular Degeneration? American Macular Degeneration Foundation.
- Boyd K, Turbert D. Eye Anatomy: Parts of the Eye and How We See. American Academy of Ophthalmology. March 9, 2021.
- Pennington KL, DeAngelis MM. Epidemiology of Age-Related Macular Degeneration (AMD): Associations With Cardiovascular Disease Phenotypes and Lipid Factors (PDF). Eye and Vision. December 22, 2016
- Age-Related Macular Degeneration (AMD) Data and Statistics. National Eye Institute. July 17, 2019.
- Dry Macular Degeneration. BrightFocus Foundation.
- View How Macular Degeneration May Affect Vision. BrightFocus Foundation. October 29, 2018.
- Stargardt Disease Defined. The American Macular Degeneration Foundation.
- Stargardt Disease. Foundation Fighting Blindness.
- Boyd K. Stargardt Disease Symptoms. American Academy of Ophthalmology. April 23, 2020.
- What Is Stargardt Disease? National Eye Institute. July 10, 2019.
- García-Layana A, Cabrera-López F, García-Arumí J, et al. Early and Intermediate Age-Related Macular Degeneration: Update and Clinical Review. Clinical Interventions in Aging. October 3, 2017.
- Risk Factors for Macular Degeneration. American Macular Degeneration Foundation.
- Wet Macular Degeneration — Symptoms and Causes. Mayo Clinic. December 11, 2020.
- Wet Macular Degeneration — Diagnosis and Treatment. Mayo Clinic. December 11, 2020.
- Age-Related Macular Degeneration (AMD): Overview. InformedHealth.org. May 3, 2018
- Boyd K. How Is AMD Diagnosed and Treated? The American Academy of Ophthalmology. February 28, 2020.
- Photodynamic Therapy for Age-Related Macular Degeneration. Johns Hopkins Medicine.
- Macular Degeneration Treatments. American Macular Degeneration Foundation.
- Age-Related Macular Degeneration (AMD). Johns Hopkins Medicine.
- Age Related Eye Disease Studies AREDS/AREDS2. National Eye Institute. April 13, 2020.
- Duffy MA. What Is Low Vision? VisionAware.
- Ultra-Violet and Blue Light Aggravate Macular Degeneration. American Macular Degeneration Foundation.
- Cimarolli VR, Casten RJ, Rovner BW, et al. Anxiety and Depression in Patients With Advanced Macular Degeneration: Current Perspectives. Clinical Ophthalmology. December 30, 2015.
- Charles Bonnet Syndrome. Macular Society.
- Fisher DE, Klein BEK, Wong TY, et al. Incidence of Age-Related Macular Degeneration in a Multi-Ethnic United States Population: The Multi-Ethnic Study of Atherosclerosis. Ophthalmology. February 16, 2016.
- Merle BMJ, Colijn JM, Cougnard-Grégoire A, et al. Mediterranean Diet and Incidence of Advanced Age-Related Macular Degeneration. Ophthalmology. March 1, 2019.
- Cataracts. National Eye Institute. August 3, 2019.



































